Constipation is one of the most common digestive complaints—yet it’s rarely talked about in depth or treated at the root. If you’ve ever struggled with bloating, discomfort, infrequent bowel movements, or the frustration of “doing everything right” and still feeling backed up, you’re not alone. Constipation isn’t just about irregular bathroom habits—it’s a signal that something deeper may be going on in your gut, hormones, nervous system, or lifestyle. In this blog, we’ll dive deep into the science behind constipation, the gut microbiome, absorption, key markers like zonulin and indican, and how lifestyle, stress, and diet all play a role. You’ll also learn about powerful tools like probiotics, prebiotics, gut repair strategies, and how short-term fasting can help restore balance. Whether you’re looking for long-term relief or a deeper understanding of your body, this guide will give you the clarity and tools to take control of your digestive health.
How Gut Health, Hormones, and Lifestyle Are All Connected
Constipation is more than just an uncomfortable inconvenience—it’s a signal that something deeper may be off in your gut, your hormones, or even your nervous system. With rising rates of digestive issues, it’s time we look beyond surface-level solutions and dig into the root causes. This blog will walk you through why constipation happens, how the gut works, and exactly what you can do to support healthy, regular digestion from a whole-body perspective.
What Is Constipation, Really?
Constipation is defined as having fewer than three bowel movements per week, or passing hard, dry, and difficult-to-eliminate stools. But true digestive health is about more than frequency—it’s about ease, timing, and full elimination. Constipation may include:
- Straining to go
- A sensation of incomplete evacuation
- Bloating or abdominal discomfort
- Gas and low appetite
Understanding the Gut Microbiome
Your gut is home to trillions of bacteria, viruses, and fungi that form your gut microbiome. These microorganisms play a key role in digestion, immune regulation, hormone metabolism, brain function, and nutrient absorption.
The gut microbiome is one of the most fascinating and vital systems in the human body. It refers to the trillions of microorganisms—bacteria, viruses, fungi, and other microbes—that live primarily in your large intestine. These tiny organisms may be microscopic, but they play an enormous role in your overall health. Your microbiome is responsible for aiding digestion, producing key vitamins, regulating the immune system, influencing mood and brain function, and even helping to balance hormones. Think of it as a living ecosystem inside your body that constantly communicates with your brain, nervous system, and immune cells.
A healthy, diverse microbiome helps maintain regular bowel movements, produces short-chain fatty acids (SCFAs) to reduce inflammation, and protects your gut lining from harmful pathogens. On the other hand, an imbalanced microbiome—known as dysbiosis—can contribute to constipation, bloating, brain fog, fatigue, and even anxiety or depression. This is because about 70% of your immune system resides in your gut, and over 90% of serotonin (a key mood-regulating neurotransmitter) is produced there too.
Your microbiome is shaped by many factors including birth method, diet, antibiotic use, stress levels, and overall lifestyle. The more diverse your microbial environment, the more resilient your gut becomes. That’s why nurturing your microbiome with the right foods, habits, and stress management techniques is one of the most effective ways to support long-term digestive and overall health.
Types of Gut Bacteria:
- Beneficial (commensal) bacteria: Bifidobacterium, Lactobacillus, Akkermansia
- Opportunistic bacteria: Can overgrow and cause symptoms if not kept in check (e.g., Klebsiella, Clostridium)
- Pathogenic bacteria and yeast: Can cause inflammation, permeability, and symptoms like constipation when present in high amounts (e.g., Candida, E. coli strains)
Maintaining a balanced microbiome is essential for motility, stool formation, and the communication between the gut and brain.
Why Does Constipation Happen?
Constipation is more than just an occasional inconvenience—it’s often a sign that something deeper is going on within your body. At its core, constipation occurs when the digestive system slows down and waste moves too slowly through the colon, causing stools to become hard, dry, and difficult to pass. But what actually causes this slowdown? The answer isn’t always simple. Constipation is typically a symptom of multiple overlapping issues, including poor diet, dehydration, hormonal imbalances, gut dysbiosis, stress, and nervous system dysfunction.
In many cases, constipation reflects an imbalance in the gut-brain axis—the communication network between your digestive system and central nervous system. When stress levels are high, or when the nervous system is stuck in “fight or flight” mode, the digestive system can become sluggish. Additionally, a lack of fiber, healthy fats, or adequate hydration can make it harder for the body to form and move stool properly. Gut bacteria also play a critical role in regulating motility. An imbalance in your microbiome can slow down digestion and increase the likelihood of hard, infrequent bowel movements.
Hormones matter, too. Women often experience constipation during times of hormonal fluctuation—such as before menstruation, during pregnancy, or in perimenopause—because progesterone and estrogen directly influence bowel function. Similarly, low thyroid function can reduce gut motility. Constipation can also be a sign of inflammation, gut permeability (leaky gut), or poor absorption, which affects how nutrients and water are processed in the intestines.
Understanding why constipation happens is the first step in correcting it—not just temporarily, but for good. By identifying the root causes and supporting your gut through nutrition, lifestyle shifts, and targeted strategies, you can restore regularity and protect your long-term digestive health.
Constipation can have many causes—often a mix of diet, stress, hormones, and lifestyle factors. Here’s what may be contributing:
1. Poor gut motility
- Caused by low fiber, dehydration, or imbalanced gut bacteria
2. Gut permeability (“Leaky Gut”)
- When the gut lining is compromised, it can affect absorption and immune response
3. Inflammation
- Systemic or localized inflammation slows digestion and impairs motility
4. Hormonal changes
- Estrogen, progesterone, cortisol, and thyroid hormones all impact digestion
5. Stress and nervous system dysregulation
- The gut is deeply connected to the brain via the vagus nerve. High stress = slow motility.
Gut Absorption and the Role of the Intestinal Wall
Gut absorption is one of the most critical functions of your digestive system—and it all takes place along the delicate and highly intelligent structure of the intestinal wall. Once food is broken down into its smallest components—amino acids, fatty acids, simple sugars, vitamins, and minerals—it’s the job of the small intestine to absorb these nutrients into the bloodstream so they can nourish every cell in your body. This process happens across the intestinal lining, a single layer of tightly packed cells designed to allow nutrients in while keeping harmful substances out.
The intestinal wall is covered in millions of tiny, finger-like projections called villi and microvilli, which dramatically increase the surface area for nutrient absorption. These structures are equipped with enzymes and transporters that selectively allow digested nutrients to pass through into your circulation. Just beneath this layer lies the gut-associated lymphoid tissue (GALT)—a key part of the immune system that monitors what’s coming through and protects the body from harmful invaders.
However, when the gut lining becomes damaged—due to chronic inflammation, stress, infections, or poor diet—this highly selective barrier can become compromised. This is known as gut permeability, or “leaky gut.” When this happens, undigested food particles, toxins, and bacteria can slip through the gaps in the lining and enter the bloodstream, triggering immune responses and widespread inflammation.
Impaired absorption not only leads to nutrient deficiencies, fatigue, and skin issues, but it also contributes to constipation. When the body isn’t absorbing water properly or processing food efficiently, stool can become dry, compacted, and difficult to pass. Additionally, damage to the gut lining often disrupts enzyme production and motility, further slowing digestion.
Supporting gut absorption means protecting and healing the intestinal wall. This can be done by reducing inflammatory foods, managing stress, rebuilding gut flora, and providing the nutrients the gut lining needs to repair—like glutamine, zinc, collagen, and omega-3s. When your intestinal wall is strong and your absorption is efficient, your digestion—and your overall health—can thrive.
The small intestine is where nutrients are absorbed after food is broken down. A single layer of cells forms the intestinal lining, allowing nutrients to pass into the bloodstream while keeping out harmful substances.
When the gut lining becomes too permeable, it can lead to malabsorption, immune dysfunction, and inflammation.
Zonulin and Indican: Two Key Gut Markers
Zonulin and indican are two important markers that provide insight into the health of your gut—and they can help explain why you may be experiencing symptoms like constipation, bloating, food sensitivities, fatigue, or brain fog. These markers are especially valuable because they go beyond basic digestion and reveal what’s happening on a deeper, functional level in your gut lining and microbiome.
Zonulin: The Gatekeeper of Gut Permeability
Zonulin is a protein that regulates the tight junctions between cells in your intestinal wall. These tight junctions act like tiny gates, opening and closing to allow properly digested nutrients into the bloodstream while keeping out harmful substances. When zonulin levels rise, it signals that these gates are being held open too long or too often—a condition known as increased gut permeability, or more commonly, leaky gut.
A leaky gut allows undigested food particles, toxins, and bacteria to slip through the gut lining and enter the bloodstream. This can trigger chronic inflammation, immune reactions, hormone disruption, and digestive symptoms—constipation included. Elevated zonulin levels are often seen in people with autoimmune conditions, food intolerances (like gluten sensitivity), and chronic gut inflammation.
Indican: A Marker for Protein Fermentation and Dysbiosis
Indican (also known as urinary indican or indoxyl sulfate) is a compound produced when protein is improperly broken down and fermented by gut bacteria. Elevated indican levels suggest an imbalance in the microbiome—typically an overgrowth of harmful or opportunistic bacteria—and poor protein digestion. This process creates toxic byproducts that can irritate the gut lining, slow motility, and contribute to symptoms like bloating, brain fog, bad breath, and—you guessed it—constipation.
High indican is often a red flag for gut dysbiosis, slow transit time, and compromised digestion. It can also point to low stomach acid or enzyme deficiency, both of which impair the breakdown of food in the stomach and small intestine, causing it to sit too long and ferment in the colon.
Why These Markers Matter
Together, zonulin and indican help paint a clearer picture of what’s going wrong in your digestive system. Zonulin reveals how well your gut barrier is functioning, while indican reflects how balanced your gut bacteria are and how efficiently you’re breaking down protein. When both are elevated, it often indicates a leaky, inflamed, and imbalanced gut—one that’s not moving waste properly or supporting optimal health.
Monitoring these markers (typically through functional lab testing) allows practitioners to create targeted, individualized plans to heal the gut lining, rebalance bacteria, and restore healthy digestion. Addressing elevated zonulin and indican levels is a key part of any gut-healing protocol—and a powerful step toward resolving chronic constipation and other digestive complaints at the root.
Zonulin
Zonulin is a protein that regulates tight junctions in the gut lining. High zonulin levels are a marker of increased gut permeability (leaky gut). When zonulin is elevated, harmful bacteria and food particles may “leak” into the bloodstream, triggering inflammation.
Indican
Indican is a marker of protein fermentation in the gut. Elevated indican suggests dysbiosis (imbalance of bacteria) and slow transit time—common with constipation. High indican levels may lead to:
- Bloating
- Gas
- Bad breath or body odor
- Poor nutrient absorption
Gut Permeability & Constipation: What’s the Connection?
Constipation and gut permeability are more closely connected than most people realize. While constipation is often viewed as a simple issue of “not going enough,” it’s actually a sign that deeper dysfunction may be happening within the gut lining. The health of your intestinal wall—specifically its permeability—plays a major role in how smoothly your digestive system operates.
Gut permeability, often referred to as “leaky gut,” occurs when the tight junctions between cells in the intestinal lining become compromised, allowing undigested food particles, toxins, and bacteria to pass through into the bloodstream. This triggers inflammation, disrupts immune function, and alters the communication between the gut and brain. When the gut is inflamed and the lining is damaged, motility slows down, meaning the movement of food and waste through the digestive tract becomes sluggish—leading to harder stools, gas, bloating, and constipation.
Constipation itself can also worsen permeability. When waste sits in the colon too long, it can ferment and release toxins that irritate the gut lining further, creating a vicious cycle of inflammation, dysbiosis, and poor elimination. This two-way relationship makes it essential to address both constipation and gut permeability at the same time. Supporting gut integrity through proper nutrition, hydration, stress management, and targeted gut-healing protocols can help break the cycle and restore regular, healthy bowel movements.
When the gut becomes permeable:
- Inflammation increases
- Immune cells are triggered
- Digestive enzymes may not be released properly
- Bacterial balance is disrupted
All of this leads to sluggish digestion and constipation.
Lifestyle Factors That Impact Gut Function and Constipation
Gut permeability—commonly known as “leaky gut”—doesn’t just happen overnight. It’s the result of a combination of lifestyle factors that slowly wear down the protective barrier of the intestinal lining. While genetics may play a role, it’s our daily habits—what we eat, how we manage stress, how we sleep, and even how we move—that have the biggest influence on gut integrity. Over time, these choices can either strengthen the gut lining or break it down, leading to increased permeability, inflammation, and digestive symptoms like constipation, bloating, and food sensitivities.
One of the biggest contributors to increased gut permeability is chronic stress. When the body is in a constant state of “fight or flight,” it diverts energy away from digestion and reduces blood flow to the gut, impairing repair processes. High cortisol levels, often triggered by unrelenting stress, have been shown to weaken tight junctions in the intestinal wall, making it easier for harmful substances to pass through.
Diet plays a critical role as well. Ultra-processed foods, refined sugar, alcohol, gluten, and inflammatory seed oils (like soybean or canola oil) can irritate the gut lining and feed the wrong types of bacteria. A lack of dietary fiber and plant diversity can also reduce microbial diversity, which is key for maintaining gut health. Food sensitivities—especially if undetected—can further trigger immune responses that damage the gut lining over time.
Sleep deprivation and poor circadian rhythm disrupt the body’s ability to heal and regenerate tissue, including the gut lining. Sleep is when a lot of cellular repair occurs, and without enough of it, the intestinal barrier remains compromised. Additionally, sedentary behavior can slow motility and reduce circulation to the digestive tract, while overuse of medications like NSAIDs and antibiotics can strip away beneficial bacteria and damage gut tissue.
By recognizing and addressing these lifestyle triggers, we can begin to restore the integrity of the gut lining and improve overall digestion. The good news? Every positive change you make—whether it’s improving your diet, managing stress, or getting better sleep—helps your gut rebuild and function more efficiently. Healing starts with the daily choices you make.
Your gut responds to everything you do—not just what you eat.
Lifestyle Factors That Can Lead to Constipation:
- Low-fiber, processed food diet
- Inadequate hydration
- Sedentary lifestyle
- Chronic stress
- Poor sleep quality
- Irregular eating habits
- Ignoring the urge to go
- Overuse of antibiotics or medications
Probiotics & Prebiotics: What You Need to Know
Probiotics and prebiotics are two of the most important tools for maintaining a healthy gut—and they work best when used together. While they’re often talked about in the same breath, they each play very different but complementary roles in supporting digestion, immune function, and overall well-being. When it comes to constipation, bloating, inflammation, and even mood imbalances, understanding how probiotics and prebiotics work can make a significant difference in your gut health journey.
Probiotics: The Beneficial Bacteria
Probiotics are live microorganisms—mostly bacteria, but also beneficial yeasts—that provide health benefits when consumed in the right amounts. These “good bacteria” colonize your gut and help keep harmful bacteria, yeast, and pathogens in check. They also play a direct role in producing important compounds like short-chain fatty acids (SCFAs), vitamins (such as B12 and K2), and neurotransmitters like serotonin and dopamine. Certain probiotic strains can improve gut motility, soften stools, reduce inflammation, and support a healthy immune response. In short, probiotics help restore and maintain balance within your gut microbiome.
However, probiotics are not one-size-fits-all. Different strains have different functions, and not all are effective for every condition. For example, Lactobacillus rhamnosus may support immune function, while Bifidobacterium lactis may help relieve constipation and improve stool frequency.
Prebiotics: The Fuel for Your Gut Bacteria
Prebiotics, on the other hand, are non-digestible fibers that act as food for your beneficial gut bacteria. Found naturally in many plant-based foods, prebiotics help probiotics thrive, grow, and produce beneficial byproducts—like SCFAs—that nourish the gut lining and reduce inflammation. Without a steady supply of prebiotic fibers, even the best probiotics may struggle to survive and populate your gut long-term.
Prebiotics not only promote microbial diversity, but they also help regulate bowel movements, improve mineral absorption, and support overall gut integrity. They’re particularly helpful for constipation because they encourage the growth of bacteria that support peristalsis (the wave-like motion that moves waste through the digestive tract).
Synbiotic Power: Why They Work Better Together
The most effective gut-healing strategies often include both probiotics and prebiotics—this combination is called synbiotics. Think of it this way: probiotics are the seeds, and prebiotics are the fertilizer. When taken together, they create a nurturing environment that supports microbial balance, reduces harmful bacteria, and enhances the gut’s ability to digest food, absorb nutrients, and eliminate waste efficiently.
By understanding and incorporating both probiotics and prebiotics into your diet and lifestyle, you can take a powerful step toward relieving constipation, restoring gut health, and supporting your immune, hormonal, and mental health all at once.
Probiotics:
Live microorganisms that provide health benefits when consumed in adequate amounts. They help:
- Restore healthy gut flora
- Support immune function
- Improve stool consistency and frequency
Common probiotic strains:
- Lactobacillus acidophilus
- Bifidobacterium longum
- Saccharomyces boulardii
Prebiotics:
Non-digestible fibers that feed beneficial gut bacteria. Found in plant-based foods, they help maintain balance in the microbiome.
Foods Rich in Prebiotics:
- Garlic
- Onions
- Leeks
- Asparagus
- Bananas (slightly green)
- Chicory root
- Jerusalem artichokes
- Oats
Foods Containing Probiotics:
- Yogurt with live cultures
- Kefir
- Sauerkraut
- Kimchi
- Miso
- Tempeh
- Kombucha
Incorporating both prebiotic and probiotic foods supports microbial diversity and improves digestion.
The Impact of Constipation on the Body
Constipation doesn’t just affect your gut—it impacts your whole system.
Constipation doesn’t just affect your bathroom habits—it can impact nearly every system in your body. When waste sits in the colon for too long, it becomes harder, drier, and more difficult to pass, but the consequences go far beyond discomfort or bloating. Constipation can disrupt digestion, impair detoxification, throw off hormone balance, increase inflammation, and even affect your mood, energy, and immune system. It’s a sign that your body’s natural rhythm is out of sync and that something deeper may need attention.
One major issue with chronic constipation is that it slows your body’s ability to detoxify. The colon is one of your primary elimination pathways, helping you get rid of excess hormones (like estrogen), toxins, and metabolic waste. When bowel movements are infrequent, these substances can be reabsorbed into the bloodstream, putting extra strain on the liver and leading to symptoms like hormonal imbalance, headaches, skin breakouts, and fatigue. This is especially important for women, as estrogen dominance can be made worse by poor elimination.
Constipation also affects your gut microbiome. When waste stagnates in the colon, it creates an environment where harmful bacteria and yeast can thrive, leading to dysbiosis and increased production of gas, toxins, and inflammatory compounds. This can weaken the intestinal lining, contributing to leaky gut, and trigger immune system reactions, food sensitivities, or systemic inflammation.
On a hormonal level, constipation often reflects or worsens cortisol imbalances. Cortisol, your main stress hormone, plays a significant role in gut motility. If you’re under chronic stress, cortisol levels may be too high or too low, both of which can slow digestion. This stress-gut connection also impacts the nervous system, as the gut and brain are constantly communicating. Constipation can worsen feelings of anxiety or depression and may even lead to a sense of mental fog or sluggishness.
Finally, constipation has a direct impact on weight management. A sluggish gut can slow metabolism, increase water retention, and disrupt blood sugar regulation. When digestion is off, the body tends to store rather than burn, and this can make weight loss frustrating—even when you’re eating well.
In short, constipation is more than a digestive issue—it’s a full-body issue. Understanding the far-reaching effects of slow elimination can help you see why addressing it is so important for your overall health, energy, and long-term wellness.
1. Cortisol & Stress
Straining, bloating, and feeling “off” can raise cortisol. Chronically elevated cortisol affects digestion, sleep, and weight regulation.
Cortisol and gut health have a powerful two-way relationship—each one directly impacts the other. Cortisol, your primary stress hormone, is produced by the adrenal glands in response to physical, emotional, or environmental stress. While cortisol is essential for survival—it helps regulate blood sugar, inflammation, and energy—chronic elevations or imbalances can wreak havoc on your gut.
When cortisol levels are too high for too long, the body stays in a state of “fight or flight”, which slows down digestion and impairs gut motility. Blood is diverted away from the digestive tract to prioritize muscles and the brain, reducing the production of stomach acid, digestive enzymes, and bile, all of which are necessary for breaking down food and absorbing nutrients. This can lead to bloating, constipation, nutrient deficiencies, and even the overgrowth of harmful bacteria.
Elevated cortisol also contributes to increased intestinal permeability (leaky gut) by weakening the tight junctions in the gut lining. This allows undigested food particles, toxins, and pathogens to enter the bloodstream, triggering inflammation and immune responses. Over time, this chronic inflammation can worsen digestive issues and place even more stress on the adrenal glands, creating a vicious cycle of stress and gut dysfunction.
On the flip side, a poor-functioning gut can dysregulate cortisol production. When the microbiome is imbalanced, or when the gut lining is inflamed or leaky, the body perceives it as a chronic internal stressor. This keeps the hypothalamic-pituitary-adrenal (HPA) axis activated, leading to dysregulated cortisol patterns—like elevated nighttime cortisol (which disrupts sleep) or flattened cortisol throughout the day (which causes fatigue and brain fog).
Whether cortisol is too high or too low, the gut feels the effects. That’s why it’s crucial to support both systems together. Calming the nervous system through stress-reduction techniques, balancing blood sugar, and healing the gut lining can all help normalize cortisol levels—and in turn, restore healthy digestion, mood, and energy.
2. Hormonal Disruption
Poor elimination means estrogen can recirculate, contributing to PMS, bloating, and weight gain.
Hormones and gut health are deeply interconnected, and when the gut isn’t functioning properly, it can throw your entire hormonal system out of balance. Your digestive system plays a key role in producing, activating, and eliminating hormones—so when gut health is compromised, hormone regulation suffers.
One of the most significant ways this shows up is through impaired estrogen detoxification. After estrogen has been used in the body, it’s sent to the liver for processing and then to the gut for elimination. If you’re constipated or your microbiome is out of balance, that estrogen can get reabsorbed into the bloodstream, leading to a condition called estrogen dominance. This can cause symptoms like PMS, heavy periods, bloating, weight gain (especially around the hips and abdomen), mood swings, and even increase the risk for hormone-driven conditions like fibroids or endometriosis.
The gut also influences thyroid function, which directly affects metabolism, energy, and digestion. Poor gut health can contribute to sluggish thyroid hormone conversion (from T4 to active T3), worsening constipation and fatigue. Leaky gut, in particular, is a known trigger for autoimmune thyroid conditions like Hashimoto’s.
Additionally, over 90% of serotonin, a neurotransmitter that influences mood, sleep, and appetite, is produced in the gut. When your gut is inflamed or imbalanced, serotonin production may decrease, leading to mood disorders, sleep disruption, and cravings—all of which can further disrupt hormone balance.
Cortisol, your main stress hormone, also plays a role. Chronic gut issues act as internal stressors, raising cortisol and keeping the body in “fight or flight” mode. Over time, this can suppress reproductive hormones (like progesterone and testosterone), interfere with ovulation, and worsen symptoms of perimenopause or menopause.
In short, hormones can’t thrive without a healthy gut. Addressing digestion, supporting the microbiome, and ensuring proper elimination are essential steps for achieving hormonal balance and feeling your best at every stage of life.
3. Immune System
70% of your immune cells live in your gut. Constipation and dysbiosis can lead to low immunity and increased food sensitivities.
The health of your immune system is directly linked to the health of your gut. In fact, about 70% of your immune cells reside in your gut, specifically within the gut-associated lymphoid tissue (GALT) found in the lining of your small intestine. This means that your gut isn’t just responsible for digestion—it also acts as a first line of defense against pathogens, toxins, and anything your body perceives as a threat.
When the gut is functioning well, it serves as a tightly regulated barrier that allows nutrients to pass through while keeping out harmful invaders. But when the gut becomes inflamed or overly permeable (a condition often called leaky gut), it allows undigested food particles, toxins, and microbes to slip through the gut lining and into the bloodstream. This triggers an immune response, and over time, this chronic, low-grade inflammation can contribute to immune dysfunction.
A compromised gut can also confuse the immune system, leading it to overreact (causing allergies or autoimmune responses) or underreact (making you more vulnerable to infections). Dysbiosis—an imbalance of good and harmful bacteria in the gut—further complicates immune function. Certain beneficial bacteria, like Lactobacillus and Bifidobacterium, are essential for training the immune system to distinguish between friend and foe. Without a healthy balance of microbes, the immune system may become hyperactive or sluggish, leading to increased illness, fatigue, or inflammatory conditions.
Constipation plays a role in this immune disruption as well. When waste stays in the colon too long, it creates a toxic environment that feeds bad bacteria and puts more stress on the immune system. Proper elimination is essential for detoxification, reducing immune burden, and maintaining a healthy internal environment.
In short, your gut is the gatekeeper for your immune system. Supporting gut health through proper digestion, microbial balance, and reduced inflammation helps keep your immune system sharp, resilient, and balanced—better equipped to defend you without overreacting.
4. Nervous System
The gut-brain axis controls motility. Constipation can trigger anxiety and even depression due to impaired neurotransmitter production.
The nervous system and the gut are deeply intertwined through a complex communication network known as the gut-brain axis. This bidirectional system allows the brain and the gut to constantly send messages to each other via nerves, neurotransmitters, hormones, and the microbiome. When the gut is imbalanced or inflamed—due to constipation, leaky gut, or dysbiosis—it can have a profound effect on the nervous system, impacting mood, focus, stress levels, and overall mental well-being.
At the core of this connection is the vagus nerve, which acts like a superhighway between the brain and the digestive tract. It regulates digestion, gut motility, heart rate, and even inflammation. When gut function is disrupted, the vagus nerve’s signaling can weaken, contributing to both sluggish digestion (like constipation) and nervous system dysregulation, such as anxiety, depression, or chronic stress.
The gut also produces and regulates key neurotransmitters that affect the brain. For example:
- Serotonin: About 90% of this “feel good” neurotransmitter is made in the gut. Poor gut health can reduce serotonin production, impacting mood, sleep, and pain sensitivity.
- GABA: A calming neurotransmitter that helps reduce anxiety and promote relaxation—also influenced by gut bacteria.
- Dopamine: Involved in motivation and focus, and partially produced by certain gut microbes.
When gut function is impaired, neurotransmitter production and regulation suffer, often resulting in symptoms like brain fog, irritability, mood swings, and poor sleep. On the flip side, chronic stress or trauma—processed through the nervous system—can impair gut motility, reduce enzyme production, and disrupt the microbiome, creating a vicious cycle of gut and brain dysfunction.
Healing the gut can directly improve nervous system health by reducing inflammation, enhancing neurotransmitter function, and restoring communication between the brain and the body. Practices like deep breathing, vagus nerve stimulation, mindfulness, and gut-healing nutrition can help calm the nervous system and support long-term digestive and mental health.
5. Weight Gain
Toxin buildup, fluid retention, and poor metabolism due to constipation can make it difficult to lose weight or maintain energy.
Gut health plays a powerful and often overlooked role in weight management. When the digestive system isn’t functioning properly—whether due to constipation, poor absorption, inflammation, or an imbalanced microbiome—it can create internal roadblocks that make losing or maintaining weight much more difficult, even when you’re eating well and exercising.
One of the key ways gut health impacts weight is through inflammation. When the gut lining becomes compromised (as in leaky gut), inflammatory molecules can leak into the bloodstream, creating low-grade systemic inflammation. This inflammation affects insulin sensitivity, hormone balance, and metabolism—slowing your body’s ability to burn fat and build lean muscle. Chronic inflammation can also increase cortisol levels, your body’s main stress hormone, which encourages fat storage, particularly around the midsection.
Another major factor is hormone recycling. Estrogen and other hormones are processed by the liver and excreted through the gut. If you’re constipated or not eliminating regularly, those hormones can get reabsorbed into the bloodstream, leading to estrogen dominance—a condition that often results in weight gain, water retention, and difficulty losing fat, especially for women in perimenopause or menopause.
The microbiome also plays a central role in regulating metabolism and energy balance. Certain gut bacteria are more efficient at extracting calories from food, storing fat, and influencing hunger hormones like ghrelin and leptin. An imbalance in gut bacteria (dysbiosis) can increase cravings, disrupt blood sugar, and interfere with appetite regulation—making it harder to manage weight, even with healthy habits in place.
Nutrient absorption is another critical piece. If your gut isn’t absorbing essential nutrients properly—like magnesium, B vitamins, or protein—your metabolism can slow down, energy levels can drop, and muscle repair can be compromised. This often leads to a slower metabolism and increased fat storage.
Ultimately, a sluggish, inflamed, or imbalanced gut can make it nearly impossible for your body to operate efficiently, making weight loss frustrating and unsustainable. Supporting gut health through proper digestion, regular elimination, microbial balance, and reduced inflammation not only improves your digestion but also enhances your ability to maintain a healthy weight—naturally and effectively.
The Gut Repair Protocol
The gut repair protocol is a foundational approach to restoring digestive health and addressing a wide range of symptoms that stem from gut dysfunction—including constipation, bloating, food sensitivities, fatigue, hormonal imbalances, and even mood disorders. The gut is not only responsible for breaking down and absorbing nutrients, but also for regulating the immune system, managing inflammation, supporting detoxification, and producing neurotransmitters like serotonin. When the gut is inflamed, leaky, or imbalanced, it can throw off nearly every system in the body.
That’s where a gut repair protocol comes in—it’s designed to remove irritants, rebuild the gut lining, restore microbial balance, and optimize digestion and absorption. This approach focuses on healing the root causes of gut issues, rather than just masking symptoms.
Without a healthy gut lining, even the most nutrient-dense diet can fall short because the body simply isn’t absorbing nutrients efficiently. If you’re constantly inflamed or experiencing leaky gut, undigested food particles and toxins can pass into the bloodstream, triggering widespread inflammation, immune reactions, and worsening constipation or sluggish digestion.
A proper gut repair protocol typically includes:
- Removing inflammatory foods, pathogens, and irritants
- Replacing essential digestive support (like enzymes or stomach acid)
- Reinoculating the gut with beneficial bacteria (probiotics and prebiotics)
- Repairing the gut lining with nutrients like glutamine, zinc, collagen, and omega-3s
- Rebalancing lifestyle factors like stress, sleep, and movement
When done correctly, a gut repair protocol not only helps relieve constipation but also improves energy, mental clarity, hormone balance, immune strength, and your body’s overall ability to function and heal. It’s not just about fixing digestive symptoms—it’s about rebuilding the foundation of your entire health.
Repairing the gut is possible with a strategic approach.
1. Remove:
- Processed foods
- Sugar and excess alcohol
- Food sensitivities
- Inflammatory oils (canola, soybean, corn)
2. Replace:
- Digestive enzymes
- Stomach acid support (like betaine HCl)
- Whole foods with fiber and nutrients
3. Reinoculate:
- Add probiotics and prebiotic-rich foods
- Use targeted supplementation if needed
4. Repair:
- Use gut-healing nutrients like:
- L-glutamine
- Zinc carnosine
- Slippery elm
- Aloe vera
- Collagen
- Bone broth
24-Hour Fasts: Why They Help the Gut
Fasting has gained a lot of attention in recent years—and for good reason. While many people associate fasting with weight loss or blood sugar control, one of its most powerful and lesser-known benefits is its ability to support gut health and digestive repair. When done strategically, fasting can give your digestive system a much-needed break, allowing it to rest, reset, and heal.
During a fasting period—especially one lasting 12 to 24 hours—the body activates a process called the migrating motor complex (MMC), a series of wave-like contractions that help sweep waste, bacteria, and undigested food through the digestive tract. This internal “housekeeping” system only occurs when the body is not digesting food and plays a key role in preventing bacterial overgrowth, reducing bloating, and maintaining healthy gut motility.
Fasting also supports autophagy, a natural cellular cleanup process that helps remove damaged cells and regenerate healthy ones. In the gut, this translates to reduced inflammation, improved gut barrier function, and better microbial balance. Giving the gut a pause from constant digestion allows time for the intestinal lining to repair, which is especially helpful for those dealing with leaky gut, constipation, or chronic inflammation.
In addition, fasting can help rebalance the gut microbiome by reducing harmful bacteria and allowing beneficial bacteria to flourish. It helps regulate insulin and cortisol, two hormones that, when imbalanced, can slow digestion and contribute to constipation or dysbiosis.
Fasting doesn’t mean starving—it means creating intentional windows of eating and resting that allow your body to reset. Whether it’s a gentle 12-hour overnight fast or a longer 24-hour reset, incorporating fasting into your routine can be a powerful, natural way to promote a healthier, more resilient gut.
Fasting for 12–24 hours gives the digestive system a chance to rest, which activates the migrating motor complex (MMC)—a wave-like motion that clears out debris and undigested food.
Benefits of short-term fasting:
- Enhances autophagy (cellular cleanup)
- Reduces gut inflammation
- Improves motility
- Gives the microbiome a chance to rebalance
This should be done with professional guidance if you’re struggling with blood sugar or hormone imbalances.
Dietary Strategies to Relieve Constipation
- Drink at least half your body weight in ounces of water daily
- Eat a variety of fiber sources: leafy greens, berries, flaxseeds, chia, oats
- Include magnesium-rich foods: pumpkin seeds, avocado, spinach
- Avoid dairy or gluten if they contribute to inflammation or sluggish digestion
- Add a tablespoon of olive oil or avocado oil to meals for lubrication
Sleep & Stress Reduction Strategies
Sleep and gut health are deeply connected—far more than most people realize. While it’s easy to think of digestion and rest as separate functions, the truth is that your gut and brain are in constant communication through the gut-brain axis, and sleep plays a critical role in that relationship. When sleep is disrupted, so is your digestive health.
During deep, restorative sleep, your body shifts into a parasympathetic (“rest and digest”) state, which supports digestion, nutrient absorption, detoxification, and gut lining repair. It’s also when your body produces important hormones like melatonin, which not only regulates your sleep-wake cycle but also acts as an antioxidant and anti-inflammatory agent in the gut.
Poor or insufficient sleep can throw off your circadian rhythm, a 24-hour internal clock that regulates everything from cortisol and insulin to gut motility and microbial balance. Disrupted circadian rhythms can impair the migrating motor complex (MMC), slow down digestion, increase inflammation, and contribute to constipation, bloating, and leaky gut. Additionally, poor sleep negatively affects the balance of gut bacteria—reducing beneficial strains while allowing harmful microbes to thrive.
Lack of quality sleep also raises cortisol, your main stress hormone, which can lead to slowed motility, increased gut permeability, and imbalances in your microbiome. Over time, this stress on the gut can contribute to digestive symptoms, weakened immunity, and even mood disorders like anxiety or depression.
Prioritizing quality sleep isn’t just good for energy and focus—it’s a foundational part of healing the gut. Supporting your circadian rhythm through consistent sleep and wake times, reducing screen exposure before bed, and creating a calm nighttime routine can make a powerful difference in your digestion and overall health.
Sleep:
- Go to bed and wake up at the same time daily
- Reduce screen time 1 hour before bed
- Take magnesium glycinate at night
- Create a cool, dark, quiet sleep environment
Stress has a profound impact on the gut—so much so that the digestive system is often referred to as the “second brain.” Through the gut-brain axis, your brain and gut are in constant communication, and when you’re under stress, that connection can trigger a cascade of digestive disruptions. Whether it’s chronic worry, emotional overwhelm, or physical stress like overtraining or lack of sleep, your body responds by shifting into “fight or flight” mode—a state where digestion takes a backseat.
When stress activates the sympathetic nervous system, it reduces blood flow to the gut, slows down motility, and inhibits the release of digestive enzymes and stomach acid. This can lead to symptoms like bloating, constipation, indigestion, and nutrient malabsorption. Over time, ongoing stress can also weaken the gut lining, contributing to leaky gut and increasing the risk of food sensitivities and inflammation.
Stress also alters the gut microbiome, encouraging the growth of harmful bacteria while suppressing beneficial strains. This imbalance—known as dysbiosis—can impair mood, immunity, and digestion, creating a vicious cycle where poor gut health further contributes to stress and anxiety.
Elevated cortisol, your main stress hormone, plays a key role here. While short bursts of cortisol are normal, chronic high levels can negatively impact gut permeability, enzyme function, and the balance of neurotransmitters like serotonin, 90% of which is made in the gut.
Managing stress isn’t just about mental health—it’s essential for gut health, regular digestion, and overall well-being. Incorporating stress-reducing practices like deep breathing, gentle movement, nature time, and mindfulness can help restore balance and allow your gut to function as it should.
Stress Reduction:
- Practice deep belly breathing
- Try meditation or yoga
- Spend time in nature
- Use adaptogens like Ashwagandha or Rhodiola to regulate cortisol
How to Correct Constipation: A Step-by-Step Plan
If you’re struggling with gut issues like constipation, bloating, or discomfort, it can feel overwhelming trying to figure out where to start. But the good news is—you don’t have to guess. With a personalized, root-cause approach, you can develop a targeted plan that addresses your unique needs and supports long-term digestive health.
Instead of relying on quick fixes or symptom-suppressing solutions, a comprehensive plan focuses on identifying and resolving what’s really going on—whether it’s gut dysbiosis, poor motility, food sensitivities, hormonal imbalances, or stress-related disruptions. This starts with a thorough intake of your symptoms, lifestyle, and health history, and often includes functional lab testing to uncover what’s happening beneath the surface.
From there, your plan may include strategic dietary changes, specific supplements like probiotics or gut-repair nutrients, stress-reduction techniques, sleep support, and guidance on hydration, movement, and eating habits. The goal isn’t just to relieve symptoms—it’s to create lasting change by healing the gut, improving elimination, and restoring balance throughout the body. With the right tools and guidance, you can rebuild a healthier, more resilient gut and feel your best again.
- Hydrate with filtered water, herbal teas, and mineral-rich broths
- Increase fiber gradually, aiming for 25–35g daily
- Eat probiotic & prebiotic-rich foods daily
- Move your body—walking, squats, and stretching all help gut motility
- Prioritize gut repair nutrients if dealing with leaky gut or inflammation
- Manage stress to regulate the gut-brain connection
- Establish a consistent bathroom routine—try sitting at the same time daily
- Use magnesium citrate or oxide if needed temporarily to relieve constipation
- Avoid over-reliance on laxatives, which can weaken your natural motility
- Track your bowel movements—frequency, consistency, and ease
How Food Sensitivities Impact the Gut and Immune System
Food sensitivities are often an overlooked contributor to chronic gut issues, inflammation, and immune dysfunction. Unlike food allergies, which trigger an immediate and often severe immune reaction (like hives or anaphylaxis), food sensitivities cause a delayed inflammatory response—hours or even days after eating the offending food. These reactions are subtle but powerful, and they can quietly damage the gut lining, disrupt digestion, and overactivate the immune system over time.
When you consistently consume foods your body is sensitive to, it can lead to chronic activation of immune pathways. This prolonged inflammation irritates the intestinal lining, increasing gut permeability (commonly called leaky gut), and allowing more partially digested food particles and toxins to enter the bloodstream. In turn, this keeps the immune system on high alert, contributing to a cycle of inflammation, fatigue, brain fog, constipation, bloating, skin issues, joint pain, and more.
Food sensitivities can also weaken the gut microbiome by triggering inflammatory responses that damage beneficial bacteria and allow opportunistic microbes to thrive. Over time, the immune system becomes overburdened, and symptoms may progress into more complex issues like autoimmune flare-ups, hormone imbalances, or worsening digestive problems.
Because symptoms of food sensitivities are often delayed and widespread, they can be very difficult to identify without lab testing. That’s where the MRT (Mediator Release Test) from Oxford Biomedical Labs becomes a game-changer.
What Is the MRT Test?
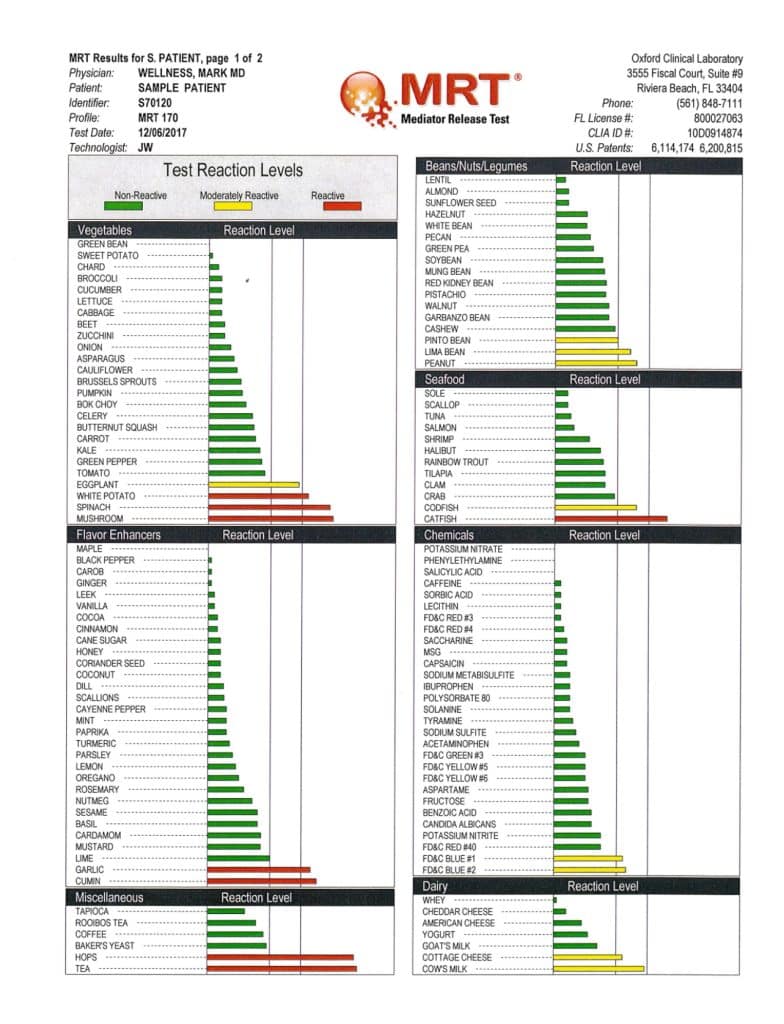
The Mediator Release Test (MRT) is a functional lab test that identifies food and chemical sensitivities by measuring the body’s inflammatory response to 170+ different foods and additives. Instead of measuring antibodies (like IgG tests), MRT measures the actual release of chemical mediators (like histamine, prostaglandins, cytokines, and more) from immune cells when exposed to specific substances.
These chemical mediators are what cause the inflammation and symptoms associated with food sensitivities. By measuring changes in the volume of your white blood cells after exposure to different foods, the MRT test can determine which foods are creating an inflammatory response in your body—even if symptoms are delayed or non-digestive.
Why MRT Is More Accurate Than Traditional Sensitivity Tests
Many food sensitivity tests on the market measure IgG antibodies, but these markers can be misleading. IgG levels may rise in response to foods you eat often—not necessarily foods that are harming you. The MRT test goes deeper by evaluating the end result of an immune reaction—inflammation—making it more reliable and clinically useful.
How Food Sensitivities Identified by MRT Impact Your Health
Once offending foods are identified and removed, people often report significant improvements in:
- Constipation and bloating
- Skin conditions (acne, eczema, rashes)
- Headaches and migraines
- Fatigue and brain fog
- Mood swings and anxiety
- Joint pain and inflammation
- Weight loss resistance
Eliminating these foods gives the gut a chance to heal, reduces inflammation in the body, and calms down an overactive immune system, helping restore balance and resilience from the inside out.
How the MRT Process Works:
- Blood draw or finger stick: Performed at home or in a lab setting.
- Lab analysis: Your sample is sent to Oxford Biomedical Labs, where it’s exposed to 170+ foods and chemicals.
- Results: Returned as a color-coded chart showing foods in green (low reactivity), yellow (moderate reactivity), and red (high reactivity).
- LEAP protocol: A certified practitioner helps you implement a personalized elimination and reintroduction plan based on your results.
The Role of Food Sensitivity Testing in a Gut Healing Protocol
For those suffering from chronic constipation, leaky gut, autoimmune symptoms, or IBS-like conditions, the MRT test offers a powerful insight into which foods may be silently contributing to the problem. Combined with other gut-healing strategies—like probiotic support, gut-lining repair, stress reduction, and proper digestion—the removal of reactive foods can rapidly reduce symptoms and accelerate healing.
In summary, food sensitivities may be the missing link in your gut and immune health journey. Identifying and removing them through advanced testing like the MRT is one of the most precise, effective ways to lower inflammation, improve digestion, and regain control of your health.
Final Thoughts: Constipation Is a Symptom, Not the Root
If you’re struggling with constipation, know that your body is communicating with you. Whether it’s stress, diet, hormones, or gut health, constipation is often the tip of the iceberg. With the right tools—testing, nutrition, mindset, and lifestyle—you can restore regularity, reduce inflammation, and feel more balanced from the inside out.
To find out more about our services that can help you achieve optimal health click here
To set up a free consultation click here


